Table of Contents
- Introduction to Person-Centered Software
- Principles of Person-Centred Care
- Benefits of Person-Centred Software
- Key Features of Person-Centred Software
- Implementation Strategies
- Challenges and Solutions
- Conclusion
Introduction to Person-Centered Software
Person-Centered Software (PCS) is a digital platform designed to enhance the quality of care provided in health and social care environments, particularly in care homes and similar settings.”Revolutionizing Care with Person-Centered Software:A Focus on Individualized Solutions” Its primary aim is to shift the focus of care from a general, one-size-fits-all approach to one that is centered on the unique needs, preferences, and well-being of each individual receiving care.
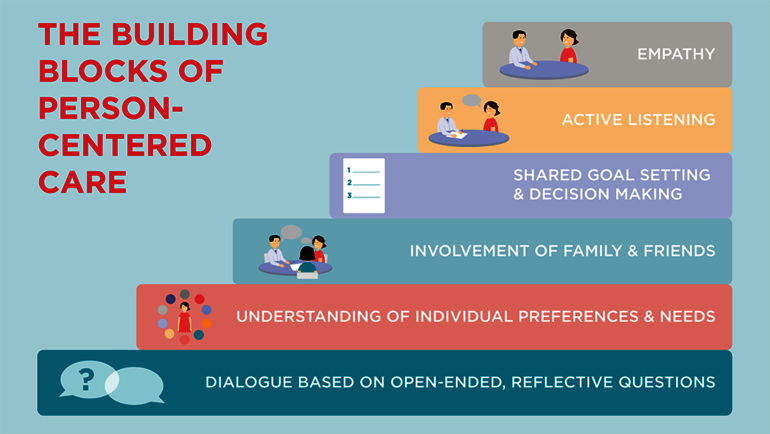
Principles of Person-Centred Care
The principles of Person-Centred Care emphasize individualized, respectful, and compassionate care, ensuring that each person’s preferences, values, and needs are at the forefront of care delivery. These principles are rooted in respect for human dignity and aim to enhance the well-being and autonomy of individuals receiving care. The key principles include:
1. Individuality
Recognizing that each person is unique, with their own life history, preferences, and needs. Care is personalized to fit the individual rather than using a one-size-fits-all approach.
2. Respect and Dignity
Ensuring that people are treated with respect, preserving their dignity, privacy, and autonomy. Every individual’s identity, beliefs, and personal choices are valued and honored.
3. Empathy and Compassion
Caregivers should demonstrate empathy and compassion, building relationships based on trust and emotional support. Understanding the emotional, psychological, and social aspects of the person is critical in providing holistic care.
4. Involvement in Care
Individuals should be actively involved in decisions about their care. Person-Centred Care encourages individuals and their families to participate in planning, setting goals, and making decisions that affect their care and well-being
5. Partnerships in Care
Person-Centred Care fosters strong partnerships between caregivers, healthcare professionals, and the person receiving care. This collaboration ensures that the person’s voice is central in shaping the care they receive.
Benefits of Person-Centred Software
The benefits of Person-Centred Software (PCS)— https://techmerge.co.uk/xtpaes in health and social care settings are numerous, focusing on enhancing both the quality of care provided and the efficiency of care management. Key benefits include:
1. Improved Care Quality
PCS enables personalized care, ensuring that individuals receive care tailored to their specific needs, preferences, and health conditions. This helps to provide a higher standard of care that promotes dignity, independence, and well-being.
2. Real-Time Monitoring and Responsiveness
Caregivers can log and monitor health information, daily activities, and any changes in condition in real time. This allows for faster response to changes in the individual’s health, helping to prevent issues from escalating.
3. Enhanced Communication and Coordination
PCS improves communication between care teams by sharing real-time information about an individual’s care needs, reducing misunderstandings and ensuring consistency in the delivery of care. This also promotes better coordination across shifts and among different caregivers.
4. Increased Efficiency and Productivity
The software reduces the time caregivers spend on paperwork and administrative tasks, allowing more time to be spent on direct care. Automated care documentation simplifies reporting and compliance, reducing the burden on staff and improving workflow.
5. Regulatory Compliance and Accurate Record Keeping
PCS helps care providers stay compliant with healthcare regulations by maintaining accurate, up-to-date records. This is especially useful for inspections, audits, and regulatory reporting, as it ensures transparency and accountability in care delivery.
Key Features of Person-Centred Software
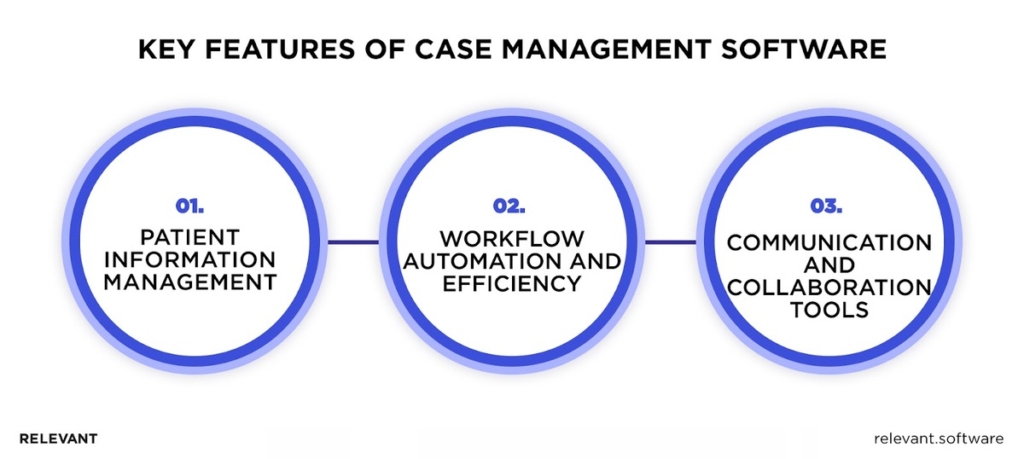
Key features typically include care planning, real-time care monitoring, communication tools for caregivers, and record-keeping, all aimed at enhancing the personal experience of care and promoting independence, dignity, and respect for the individual:
Care Planning and Assessment Tools: Enables the creation of personalized care plans and assessments, tailored to the unique needs and preferences of each individual, ensuring holistic care.
Medication Management: Streamlines the administration and tracking of medications, reducing errors and ensuring timely dosage, while keeping detailed records for compliance.
Real-Time Reporting and Monitoring: Allows caregivers to document and monitor health data and activities in real time, ensuring prompt responses to changes in a person’s condition.
Family and Resident Portals: Provides family members and residents with secure access to care updates, fostering transparency and improved communication with caregivers.
Mobile Compatibility: Allows caregivers to access and update care plans and records on-the-go through mobile devices, enhancing flexibility and efficiency in care delivery.
Implementation Strategies for Person-Centred Software (PCS) focus on ensuring smooth adoption, minimizing disruptions, and maximizing the software’s benefits in care settings.
Implementation Strategies
1. Engage Key Stakeholders Early
Involve care staff, management, IT teams, and residents (where appropriate) from the start.https://techsenc.com/crypticstreet-com-Their input helps identify key needs, ensuring the software meets practical requirements, and fosters ownership of the implementation process.
2. Comprehensive Training and Support
Offer thorough training sessions tailored to different roles, ensuring all users understand how to use the system effectively. Provide ongoing support, such as user guides, help desks, or on-site assistance, to resolve any challenges that arise during and after implementation.
3. Clear Communication Plan
Maintain open communication throughout the implementation process, keeping staff informed about timelines, goals, and the benefits of the software. Highlight how it will enhance their workflow and improve the quality of care.
Challenges and Solutions
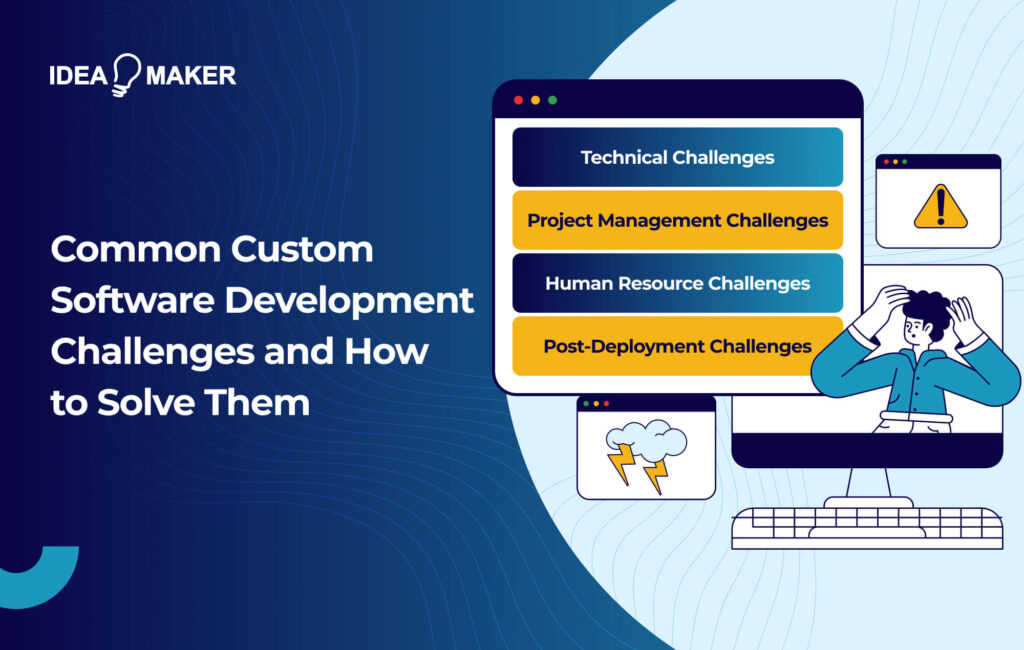
1. Challenge: Resistance to Change
Care staff may resist adopting new technology due to unfamiliarity or fear of increased workload.Solution: Provide comprehensive training and ongoing support to ensure staff understand the benefits and are comfortable using the software. Highlight how PCS can reduce manual tasks and improve care quality.
Care staff may resist adopting new technology due to unfamiliarity or fear of increased workload.
Solution: Provide comprehensive training and ongoing support to ensure staff understand the benefits and are comfortable using the software. Highlight how PCS can reduce manual tasks and improve care quality.
2. Challenge: Data Security and Privacy
Handling sensitive patient information digitally can raise concerns about data breaches or unauthorized access.
Solution: Implement strong cybersecurity measures, including encryption, secure logins, and regular audits, ensuring compliance with regulations like GDPR or HIPAA to protect personal data.
3. Challenge: Initial Cost and Resource Investment
Implementing PCS may require significant financial investment and time for setup, training, and transition.
Solution: Demonstrate the long-term cost savings and operational efficiencies PCS can bring. Use phased implementation and explore funding options or grants to ease the initial financial burden.
Future Trends in Person-Centred Software
- Artificial Intelligence and Predictive Analytics: Future PCS platforms will likely incorporate AI to analyze large datasets and predict health risks or trends, enabling early interventions and more personalized care plans based on predictive models.
- Wearable and IoT Integration: The integration of wearable devices and Internet of Things (IoT) technology will allow continuous monitoring of vital signs, movement, and daily activities, giving caregivers real-time health insights and alerts for immediate response.
- Enhanced User Experience with Voice Assistants: Voice-activated tools and virtual assistants can streamline care documentation and communication, improving accessibility for caregivers and residents, particularly for those with mobility or visual impairments.
- Telehealth and Remote Monitoring: As telehealth grows, PCS will increasingly support remote care delivery and monitoring, making it easier to provide person-centred care even outside of traditional care facilities, such as in home settings.
- Advanced Data Security and Blockchain: With data security a growing concern, the future of PCS may see the use of blockchain technology for enhanced data protection and secure, transparent record-keeping.
Conclusion
Person-Centred Software is transforming care by placing the individual at the heart of care delivery, offering personalized and efficient care management solutions. Through real-time monitoring, better communication, and tailored care plans, PCS enhances care quality and promotes autonomy, dignity, and well-being for those receiving care. As future trends like AI, IoT, and telehealth continue to evolve, PCS will become even more effective in meeting the diverse needs of individuals while improving workflow efficiency and data management for care providers. The continued adoption and advancement of PCS are set to reshape the future of health and social care for the better.

I am a Writer and Blogger at techsensc.com If you have any query or Question contact me at:
info.techsenc@gmail.com